Palliative Care Services At Home Explained
- tmcpnet
- Jan 7
- 14 min read
When a serious illness becomes part of your life, the focus often shifts entirely to treatments and appointments. But what about the person going through it all? Palliative care at home is designed to provide that crucial layer of support, focusing on comfort, dignity, and quality of life right where you feel most at ease—your own home. It’s not about giving up; it’s about adding specialized support to help you live better, right from the day of diagnosis.
What Is Palliative Care At Home

Imagine your medical team is focused on treating your illness—the "what." The palliative care team’s job is to focus on you—the "who." Their entire mission is to relieve the symptoms and stress that come with a serious health condition, making your day-to-day life more manageable and meaningful.
This isn't a substitute for your primary medical treatment. Instead, think of it as a partnership. While your oncologist, cardiologist, or other specialist works on the disease, the palliative team helps you cope with the journey by managing pain, shortness of breath, anxiety, and so much more. This type of care is available to anyone of any age, at any stage of a serious illness.
A Common Misconception: Palliative Care Vs. Hospice
Let's clear up a major point of confusion: palliative care is not the same as hospice. It’s a common mix-up, but the distinction is incredibly important.
Hospice care is reserved for the final phase of life, typically when curative treatments have stopped. In contrast, palliative care can start the moment you're diagnosed. You can receive it alongside chemotherapy, surgery, or any other treatment intended to cure or control your illness. It works in parallel, not in place of, your primary medical care. For a more detailed breakdown, check out this excellent a guide to palliative home health that explains the difference clearly.
Receiving this support at home—whether you're in Mississauga, Brampton, or anywhere in the west GTA—makes a world of difference. It removes the burden of constant travel and allows you to be surrounded by the people and things you love, giving you a sense of control and normalcy when you need it most.
The Core Goals Of Home Palliative Care
At its heart, home palliative care is about looking at the bigger picture. It’s a holistic approach that sees you as a whole person, not just a diagnosis. The team works together to ensure your physical, emotional, and spiritual needs are all met within a coordinated plan.
This table breaks down the main objectives and what they really mean for you and your family.
Goal | What It Means For You |
|---|---|
Symptom & Pain Relief | Actively managing pain, fatigue, nausea, and other distressing symptoms to maximize daily comfort and peace. |
Emotional & Spiritual Support | Addressing the emotional toll of illness, including anxiety and depression, for both the individual and their loved ones. |
Improved Quality Of Life | Focusing on what matters most to you, helping you live as fully and comfortably as possible despite the illness. |
Coordinated Medical Care | Ensuring all your doctors and healthcare providers are aligned, creating a seamless care experience that honours your wishes. |
Family & Caregiver Support | Providing education, resources, and respite to family caregivers, empowering them to provide better support without burning out. |
Understanding these goals is a foundational step, especially when navigating the complexities of caring for a loved one.
Your In-Home Palliative Care Team

When you choose palliative care at home, you’re not just getting a single person to help out. You’re welcoming a dedicated, collaborative team into your life. This isn't just a random group of healthcare workers; they're a hand-picked team of specialists who work together, communicating constantly to provide layered, synchronized support.
Think of it like a conductor leading an orchestra. Each musician has a different instrument, but they all follow the same sheet music to create a beautiful, cohesive piece. Your in-home palliative care team operates the same way. Each member brings their unique expertise to a single, unified care plan that honours your personal wishes and goals.
This team approach ensures every part of your well-being is looked after—physical, emotional, social, and spiritual. It’s a complete support system built around you, right in the comfort of your own living room.
Who Makes Up The Core Team
While the exact makeup of your team can shift based on your needs, it’s usually built around a core group of professionals. For a family in Mississauga or Oakville, this collaborative spirit is what makes home-based palliative care so incredibly effective.
Here’s a look at the key players and what they do:
Palliative Care Doctors and Nurse Practitioners are the experts in managing symptoms. They work hand-in-hand with your family doctor to prescribe medications, adjust treatments for things like pain or nausea, and oversee your medical plan.
Nurses are often the people you'll see most. They provide direct, hands-on care, administer medications, dress wounds, and act as the crucial communication link between you, your family, and the rest of the team.
Personal Support Workers (PSWs) are there to help with the activities of daily living. That means assistance with bathing, dressing, meal preparation, and light housekeeping, which frees up your energy and helps you stay as independent as possible.
Social Workers help you and your family navigate the non-medical side of things. They can connect you with community resources, offer guidance on financial planning, provide counselling, and help set up support for caregivers.
Expanding The Circle Of Support
Beyond that core medical group, your team often grows to include other specialists who add to your overall sense of well-being. Their involvement is always based on your specific needs and what you feel would be most helpful.
A holistic approach means recognizing that comfort and quality of life extend beyond just physical symptoms. True palliative support addresses the emotional, social, and spiritual needs of both the individual and their family, creating a comprehensive network of care.
This wider circle of support can include professionals like:
Spiritual Advisors or Chaplains who provide comfort and guidance that aligns with your personal beliefs and values, offering a reassuring presence for both you and your family.
Therapists, such as physiotherapists, occupational therapists, and Registered Massage Therapists (RMTs), who focus on improving mobility, function, and physical comfort.
As you begin working with your team, especially the nurses who are so central to day-to-day care, it's good to be prepared. Knowing what to ask can make all the difference. As you move forward, you might find this list of essential questions to ask your hospice nurse helpful. And for those interested in specialized therapeutic touch, our guide on massage therapy for seniors offers some valuable insights.
The Real-World Benefits of Palliative Care at Home
Opting for palliative care in your own home is about so much more than convenience. It fundamentally changes the experience of living with a serious illness. Instead of life revolving around sterile clinic appointments and hospital corridors, care revolves around your life, in your own space.
This is a powerful shift. Suddenly, you're back in control, surrounded by the familiar comforts of your own home—the view from your window, your favourite armchair, the people you love stopping by whenever they want. It helps you hold onto a sense of normalcy when everything else feels uncertain. The focus moves from what's been lost to what can be cherished: comfort, dignity, and quality of life.
A Story of Comfort and Control
Think of a family right here in Brampton. Their father was living with a chronic lung condition, and the frequent hospital stays were becoming incredibly stressful. Every admission felt like a loss of independence—he couldn’t decide when to eat, when to sleep, or even just have a quiet moment. The constant noise and unfamiliar faces left him anxious and worn out.
When they transitioned to palliative care services at home, the difference was night and day. A nurse came to manage his breathing treatments right in his living room. A personal support worker helped him with his morning routine in his own bathroom. He was able to eat meals from his own kitchen, surrounded by his family. They weren't just visitors anymore; they were a family at home again. The care plan was built around his life, not the other way around.
The heart of home-based palliative care is making sure the medical support fits the person's values and wishes. It's about empowering someone to stay in the driver's seat of their own life, in an environment that nurtures their whole being, not just their physical symptoms.
This approach also has a very practical benefit: it dramatically cuts down on stressful, last-minute trips to the emergency room. By managing symptoms before they become a crisis, the team helps keep things stable and comfortable at home.
Real Results for the Whole Family
This isn't just about feeling good; the data backs it up. Research shows that palliative home care significantly improves patient and family satisfaction while reducing hospital admissions. Innovative programs are making this possible, and the positive effects are felt by everyone involved:
Less Stress on Caregivers: Families get the training, resources, and breaks they need, so they can offer support without burning out.
Clearer Communication: The team helps facilitate important conversations about goals and wishes, getting everyone on the same page.
Better Emotional Health: Being in a comforting, familiar space can significantly ease the anxiety and depression that often accompany serious illness.
Deeper Comfort: Specialized therapies can be brought right to the bedside. Gentle, therapeutic touch, for example, can soothe physical pain while offering profound emotional comfort. You can learn more about how this works by reading about our approach to geriatric massage therapy.
Ultimately, palliative care at home shifts the entire focus from simply managing an illness to truly living. It’s about creating a circle of support where comfort is the priority, dignity is protected, and precious time with loved ones is honoured.
How to Arrange Palliative Care Services In Your Area
Figuring out how to arrange palliative care services at home can feel like trying to navigate a maze, especially when you’re already dealing with the stress of a serious illness. The good news? For families in Brampton, Toronto, Etobicoke, and the nearby communities, there’s a clear path to getting this essential support. Let's walk through the practical steps to take the mystery out of the process and help you arrange care with confidence.
It all starts with a conversation. The very first thing you need to do is talk to your family doctor, specialist, or nurse practitioner about what's going on. In Ontario, a referral from a healthcare professional is the key that unlocks publicly funded home care services.
Don’t hold back. Be open about the challenges you or your loved one are facing, whether it's pain that won't go away, too many trips to the hospital, or the sheer exhaustion of being a caregiver. This honesty helps your doctor make a formal referral to the right place.
Connecting with Home and Community Care Support Services
Once your doctor sends the referral, the next stop is your local Home and Community Care Support Services. You might know them by their old name, the Local Health Integration Network or LHIN. This is the government agency that coordinates all the in-home healthcare for our province.
You'll be assigned a care coordinator who becomes your primary contact and guide. Think of them as your personal navigator for the healthcare system. Their job is to help you understand what services are available and to work with you to create a plan that actually fits your family’s unique situation.
Preparing for The Initial Assessment
Your care coordinator will set up an initial assessment, which almost always happens right in your home. This isn't a test—it's a conversation. The goal is to get a real-world picture of your needs, your goals, and your home environment.
To get the most out of this meeting, it helps to be prepared.
List Your Symptoms: Jot down any physical symptoms like pain, nausea, or fatigue, and try to note how severe they are.
Note Daily Challenges: Think about everyday activities. Is bathing difficult? Cooking? Just getting around the house? Mention it.
Gather Medical Information: Have a list of current medications handy, along with your Ontario Health Card (OHIP) number.
Express Your Goals: This is so important. Be clear about what you’re hoping for. Do you want to stay out of the hospital? Does the family caregiver desperately need a break?
This conversation is what determines your eligibility and exactly which services (and how much of them) you'll receive.
This chart shows some of the core benefits that a well-designed home palliative care plan can offer.
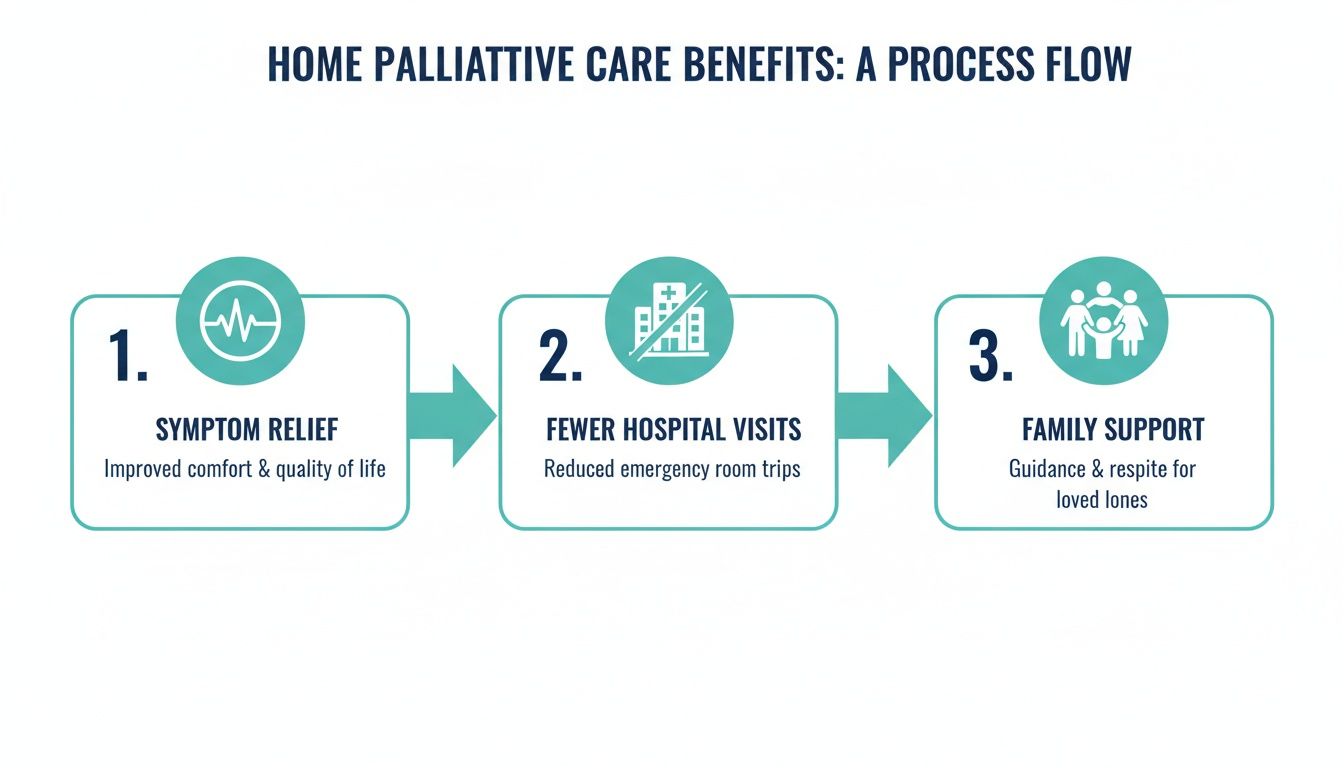
By being proactive with symptom relief and wrapping support around the entire family, the focus is always on making life at home more comfortable and avoiding those disruptive trips to the emergency room.
Understanding Funding and Coverage
One of the biggest worries for any family is, "How much will this cost?" Thankfully, in Ontario, many of the core palliative care services arranged through Home and Community Care Support Services are covered by OHIP.
This typically includes:
Nursing visits
Personal support worker services (PSWs)
Physiotherapy
Social work support
It's crucial to understand, however, that OHIP doesn't cover everything. Things like 24/7 care, some medical supplies, or complementary therapies like registered massage therapy usually come out of pocket or are covered by private health benefits. Your care coordinator will be able to tell you exactly what’s covered and what isn’t.
Despite progress, access to palliative care at home remains a challenge across Canada. A 2023 analysis by the Canadian Institute for Health Information (CIHI) found significant gaps in home-based services, although Ontario is among the provinces making strides. For a detailed breakdown, you can explore the data on access to palliative care in Canada.
As you put together your support network, you might want to add private services to fill in the gaps. For help finding qualified professionals who make house calls, our article on how to find a massage therapist at home is a great resource. By taking these steps, you can build a strong circle of care that truly enhances quality of life, right where it matters most.
Enhancing Comfort with Specialized In-Home Massage

While the medical team focuses on the clinical side of a serious illness, a truly whole-person approach to palliative care services at home needs to go deeper. This is where complementary therapies, especially specialized massage, can make a world of difference in enhancing comfort, easing distress, and improving day-to-day well-being.
Therapeutic touch isn't just a luxury; it’s a powerful, non-drug approach to managing symptoms and offering real emotional comfort. For someone in palliative care, a gentle, adapted massage can bring a kind of relief that medicine alone often can't reach. It fits perfectly with the ultimate goal of palliative care: making life as good as it can be.
This kind of care is worlds away from a typical spa massage. It demands specific training, a deep understanding of the person's medical condition, and a compassionate, trauma-informed perspective.
The Gentle Power of Geriatric and Palliative Massage
When we talk about massage for someone with a serious illness, everything revolves around safety, respect, and personalization. The techniques are gentle, modified, and always adapted to the person’s comfort level and how they're feeling that day. The focus isn't on deep muscle work but on soothing the nervous system and easing discomfort.
Our male Registered Massage Therapist (RMT), Taylor, specializes in this field. He brings his expertise and compassion directly to homes in Etobicoke, Caledon, Milton, and the surrounding areas, always working in partnership with the client’s existing palliative team.
Here’s a look at some of the specialized services he offers and how they help:
Swedish Massage: This technique uses gentle, flowing strokes to promote deep relaxation, improve circulation, and calm an anxious mind and body.
Deep Tissue Massage: Adapted for palliative clients, this involves carefully applied pressure to release chronic muscle tension and discomfort.
Cupping Therapy: Using suction cups, this therapy can help ease pain and inflammation in a gentle, non-invasive way.
Myofascial & Trigger Point Release: These techniques use gentle, sustained pressure on connective tissues and specific tense spots to relieve stiffness and pain cycles.
Geriatric Massage: Tailored specifically for seniors, this approach focuses on improving mobility, circulation, and overall comfort with exceptionally gentle techniques.
The heart of palliative massage is compassionate touch. It's a way to communicate care and comfort without needing words, helping to ease the deep sense of isolation that can come with a serious illness. This human connection can be just as healing as the physical relief it brings.
Addressing More Than Just Physical Pain
The benefits of bringing a skilled RMT into a home palliative care setting go far beyond just soothing sore muscles. The emotional and psychological lift can be equally profound.
Living with a serious illness often involves a lot of clinical, prodding touch from medical procedures. The gentle, caring touch of a massage can help someone reconnect with their body in a more positive way.
This specialized service can help:
Reduce Anxiety and Stress: Gentle massage is proven to lower levels of the stress hormone cortisol while boosting endorphins, the body's natural feel-good chemicals.
Improve Sleep Quality: By easing physical discomfort and promoting deep relaxation, massage can help people get more restorative sleep—something that's absolutely vital when coping with illness.
Ease Loneliness and Isolation: The simple act of human connection through compassionate touch provides immense emotional comfort and reassurance.
Enhance Body Awareness: It can help a person feel more comfortable and at peace in their own body, which is incredibly grounding during such an uncertain time.
For a deeper look into the positive effects of in-home massage, especially for older adults, you might find valuable insights in our article on mobile massage therapists for senior wellness.
Booking Compassionate In-Home Massage
Adding specialized massage to a palliative care plan is a simple, stress-free process. Our RMT, Taylor, brings everything needed, whether it's a professional massage table or techniques adapted for a recliner or hospital bed. The entire session is built around the client's needs and environment.
He works with families in Brampton, Mississauga, Guelph, and across the west GTA to provide a safe, respectful, and comforting experience. Every session starts with a careful conversation to understand the client's current condition, comfort levels, and goals. This ensures every treatment is just right for them.
This extra layer of support can make a real, tangible difference in a loved one's daily comfort and peace of mind. To arrange for a gentle, therapeutic in-home massage session, you can easily book an appointment online.
Still Have Questions? Let's Clear Things Up
Making decisions about palliative care often comes with a lot of questions. It's completely normal. When you're looking at this kind of support for someone you care about, you need straightforward answers.
Here are some of the most common things we hear from families in Mississauga, Halton, and the surrounding areas as they start exploring palliative care at home.
"I thought palliative care was only for the very end of life. Is that true?"
Not at all. This is probably the biggest misconception out there, and it's one that can unfortunately stop people from getting help sooner. The truth is, palliative care can be a game-changer right from the moment of a serious diagnosis. Its whole purpose is to manage symptoms and make life better while you continue with treatments meant to cure or control your illness.
Think of it less as "end-of-life care" and more as an extra, specialized layer of support that wraps around you and your family. It works in tandem with your current medical plan, focusing on bringing comfort and easing the stress of it all.
"How do we pay for home palliative care in Ontario?"
This is, understandably, one of the first questions on everyone's mind. The good news is that in Ontario, most of the core services are publicly funded. Things like visits from palliative doctors, nurses, and personal support workers are typically covered by OHIP through your local Home and Community Care Support Services agency.
That said, some things might not be covered. If you're looking for 24/7 care at home or want to include complementary therapies like registered massage therapy, you'll likely need to pay for those privately or through an extended health benefits plan. Your care coordinator is your best resource here; they can walk you through exactly what's covered and what your options are for anything extra.
"If we have palliative care at home, can we still go to the hospital?"
Yes, absolutely. Choosing home-based care doesn't mean you're cut off from the hospital. In fact, one of the main goals of the palliative team is to manage symptoms so well at home that you can avoid those stressful, last-minute trips to the emergency room.
But if a medical emergency happens or a symptom becomes too difficult to handle at home, the hospital is always there. Your palliative team will work with you to create a clear "just in case" plan. They’ll coordinate with hospital staff to make sure the transition is smooth and that everyone involved knows your care preferences.
"A well-coordinated palliative plan empowers families by preparing them for potential crises. It clarifies when to call the palliative nurse, when to visit a family doctor, and when a trip to the hospital is the right choice, ensuring decisions are made with confidence, not panic."
This kind of proactive planning is what makes great home-based care work.
"How is massage different for someone in palliative care?"
This is a fantastic question, because palliative massage has very little in common with what you'd get at a spa. A properly trained RMT, like our therapist Taylor, uses incredibly gentle and adapted techniques that are customized to how the person is feeling on that specific day.
Safety is everything. The therapist works closely with the client's medical team, avoiding any sensitive spots—like areas with fragile skin, medical devices, or tumours. They use soft pillows and bolsters to support the body in a comfortable, restful position. The goal isn't deep tissue work; it's about providing compassionate touch to ease pain, calm anxiety, and improve a person's sense of well-being.
From the length of the session to the amount of pressure used, every single detail is carefully considered to provide comfort without causing any strain.
At Stillwaters Healing & Massage, we’ve seen firsthand how much compassionate, specialized care can mean to a family. We are proud to serve communities across Brampton, Toronto, Etobicoke, Oakville, Caledon, Orangeville, Mississauga, Milton, Halton, and Guelph, bringing gentle, therapeutic massage right to your home.
To add this powerful layer of comfort to your loved one's care, you can book an in-home session with our RMT, Taylor, online.









